Six Ways to Lower Rising Health Costs for Companies
Read more

Open enrollment may be the most visible season in the benefits calendar, but it’s not the most demanding one.
Once the emails stop and the elections are finalized, something less obvious begins. Employees start using their benefits. Questions surface. Confusion appears. Medical bills arrive. And HR teams, already stretched thin from enrollment, become the default support system for everything that follows.
The post–open enrollment period doesn’t get the same attention as OE itself. But it’s often where the real strain shows up and where the gaps in a benefits strategy become impossible to ignore.
• Open enrollment doesn’t end the work; it shifts it. The period after OE exposes where understanding breaks down and where support is missing.
• HR burnout is driven by constant interruption, not lack of expertise. Acting as the default benefits help desk is unsustainable.
• Employees need guidance when they’re using benefits, not just selecting them. Education must extend beyond enrollment.
• Post-OE is an opportunity, not just a recovery period. It’s the best time to evaluate how benefits are supported year-round.
• Medefy reduces HR noise by taking questions off their plate. Employees get clarity, and HR gets time back.
Open enrollment gets all the attention.
It’s the busiest, loudest, most visible moment of the benefits year. Calendars fill up. Communications fly. Questions pour in. And when it’s finally over, HR teams breathe a collective sigh of relief.
Or at least, they try to.
Because while open enrollment may end on the calendar, the real workload often begins after enrollment closes.
This is when HR teams feel the full weight of what enrollment didn’t solve: lingering confusion, unresolved questions, and employees trying to use benefits they don’t fully understand. It’s also when burnout quietly sets in, not because benefits are broken, but because support systems aren’t built for what happens after enrollment. According to StratusHR, HR teams spend up to 40 hours each month answering benefit questions— a full workweek lost to confusion.
On paper, open enrollment can look like a success. Participation rates are solid, elections are complete, and systems are updated.
But the weeks that follow tell a different story.
Employees start receiving medical bills they don’t understand. They try to find in-network providers. They question whether a service is covered. They realize they selected a benefit they don’t know how to use. . . or didn’t select one they actually need.
And when that confusion surfaces, it almost always lands in the same place: HR’s inbox, voicemail, or Slack messages.
Instead of slowing down after OE, HR teams find themselves answering the same questions again and again. Many of those questions are nuanced, situational, or outside HR’s direct expertise. Yet HR becomes the default help desk anyway.
Over time, this constant interruption takes a toll.
Most HR teams know the benefits plan inside and out. The issue isn’t competence. It’s capacity.
Post-OE questions don’t arrive in neat batches. They interrupt meetings, derail projects, and force constant context switching. One minute it’s payroll or performance reviews; the next it’s explaining deductibles or provider networks.
Even when HR has the answer, answering the same question for the tenth time that week drains energy. And when HR doesn’t have the answer, the stress compounds.
This is how burnout builds. Not from a single busy season, but from months of being the middleman between employees, carriers, TPAs, and vendors.
The period after enrollment is when many HR leaders realize they’re still carrying the enrollment workload– just without the structure or support that existed during OE.

Most benefits education is still designed around a single moment in time.
Employees receive plan summaries, comparison charts, and emails during open enrollment. But benefits aren’t just used during enrollment; they’re used throughout the year, and more often during stressful or time-sensitive moments.
When education ends with OE, employees are left to figure things out on their own in the months that follow. That’s when confusion turns into frustration, delayed care, or poor decisions.
And every one of those moments creates friction, either for the employee, HR, or both.
True benefits understanding doesn’t happen all at once. It happens in context when someone needs help making a real decision.
The time after open enrollment is revealing.
It shows employers:
• Which benefits are confusing the members
• Where communication fell short
• How much invisible labor HR is doing to keep everything running.
Instead of treating post-OE burnout as inevitable, this is the moment to ask a different question:
Who is responsible for supporting employees after enrollment— and just how sustainable is that model?
For many organizations, the answer has quietly become “HR handles it.” But that approach doesn’t scale, and it doesn’t protect the people tasked with managing it.
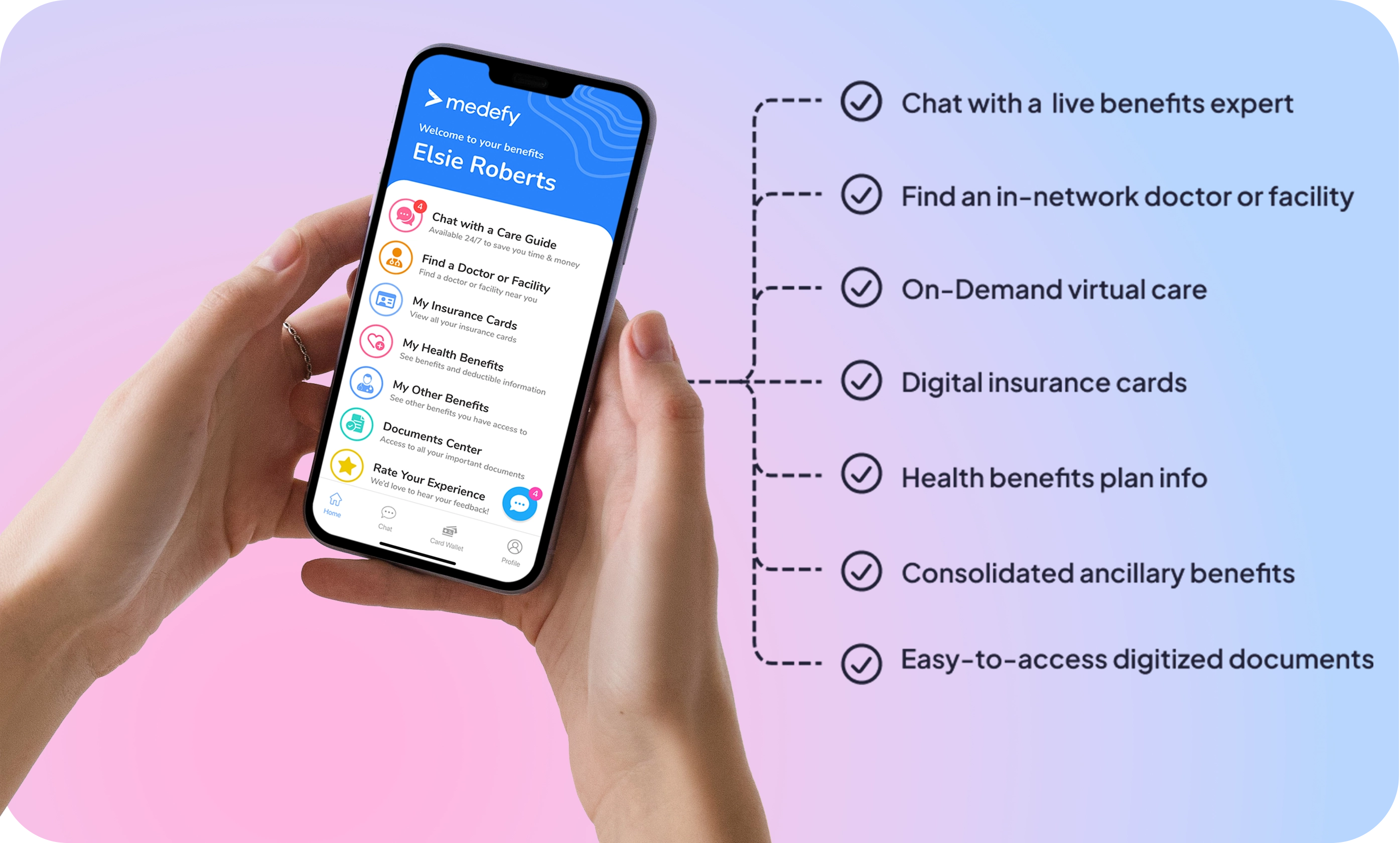
Medefy was built for what happens after open enrollment.
We don’t replace HR. We reinforce them.
By giving employees a single source of truth for their benefits and access to live Care Guides, we handle the questions that would otherwise interrupt HR’s day. Employees get clear, personalized guidance when they need it, without waiting for an email reply or escalation.
When employees know where to go:
• Questions get answered faster
• Confusion doesn’t snowball into frustration
• HR gets time and focus back
Instead of being the middleman, HR gets to step out of the constant support loop and return to higher-value work.