Six Ways to Lower Rising Health Costs for Companies
Read more

Open enrollment may be over, but for many employers, the real impact of their benefits decisions is only just becoming clear.
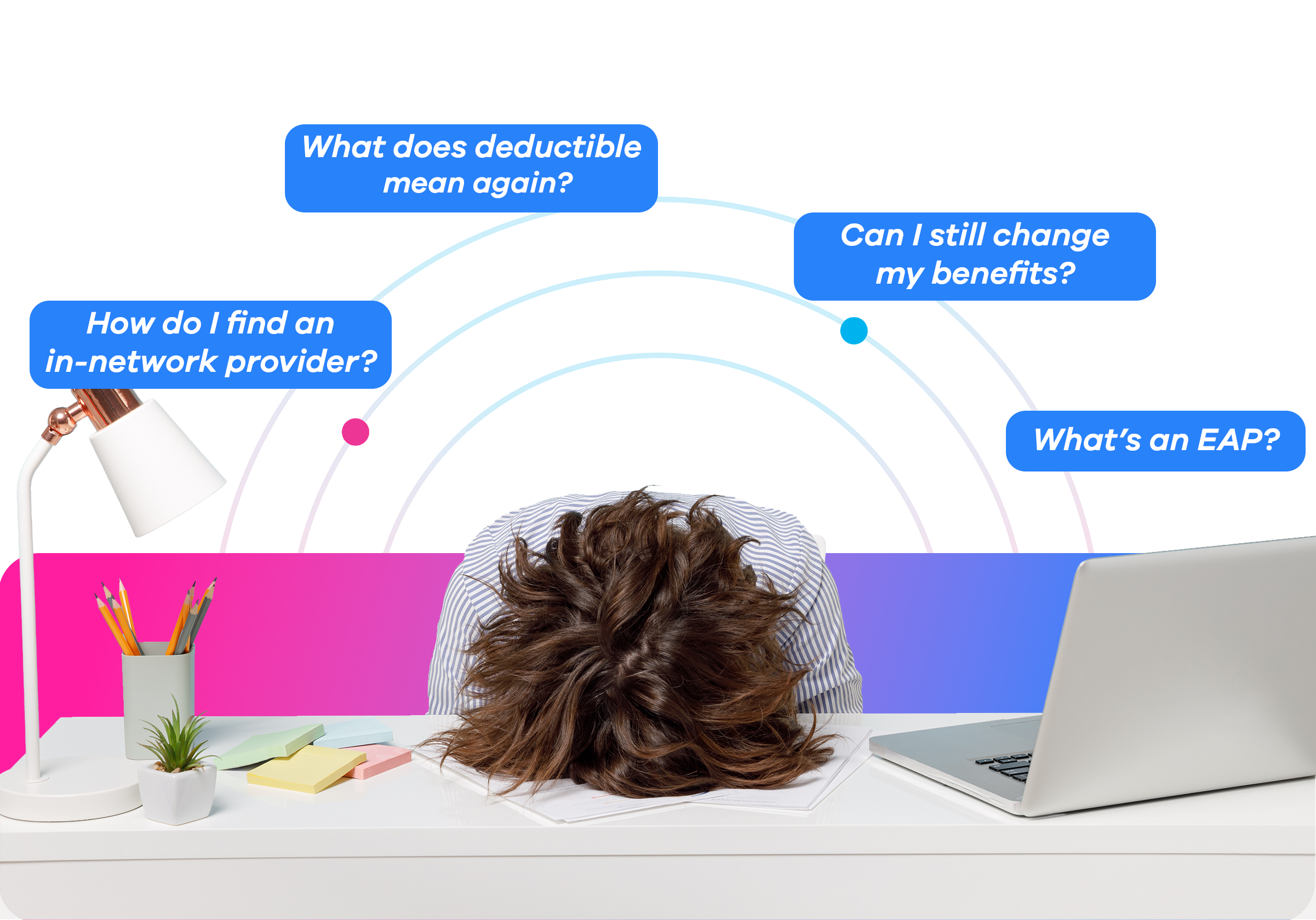
January is when participation numbers meet reality. Employees are technically enrolled, yet questions persist. Benefits go unused. HR teams find themselves fielding the same “basic” questions they thought open enrollment would solve. What looked successful on paper often reveals a deeper issue: employees selected benefits, but they don’t fully understand how to use them.
For many employers, open enrollment feels like the finish line. Elections are submitted, systems are updated, and HR teams finally come up for air after weeks of deadlines and employee questions.
But January tells a different story.
Right now is when employers and brokers begin to see what open enrollment actually delivered. . . and where it fell short. Employees are enrolled, but confusion lingers. Then, benefits are going unused. HR teams find themselves stuck answering the same questions they thought enrollment would resolve.
Participation may look strong on paper, but employees' understanding of what benefits they have (and how to use them) is a whole other matter entirely.
Research published by Business Wire shows that 73% of employees want more education about their benefits, yet post-OE administrative demands often make it difficult for HR teams to deliver ongoing support. The result is a familiar pattern: employees enroll successfully, but struggle to use their benefits throughout the year. Questions like, “Wait what’s an EAP?” or “How am I supposed to know which doctor is in-network?” start to resurface weeks or months after OE, plan engagement drops off, and HR absorbs the ongoing burden.
These aren’t edge cases; they’re a natural consequence of increasingly complex benefit ecosystems. When education is limited to a short enrollment window, comprehension rarely sticks.
The cost of this confusion goes beyond inconvenience. Employees who don’t understand their benefits are more likely to delay care, make poor decisions, or avoid using benefits altogether. Over time, that leads to higher downstream costs, lost productivity, and frustration on both sides of the desk.
This is why benefits education can’t be a once-a-year event.
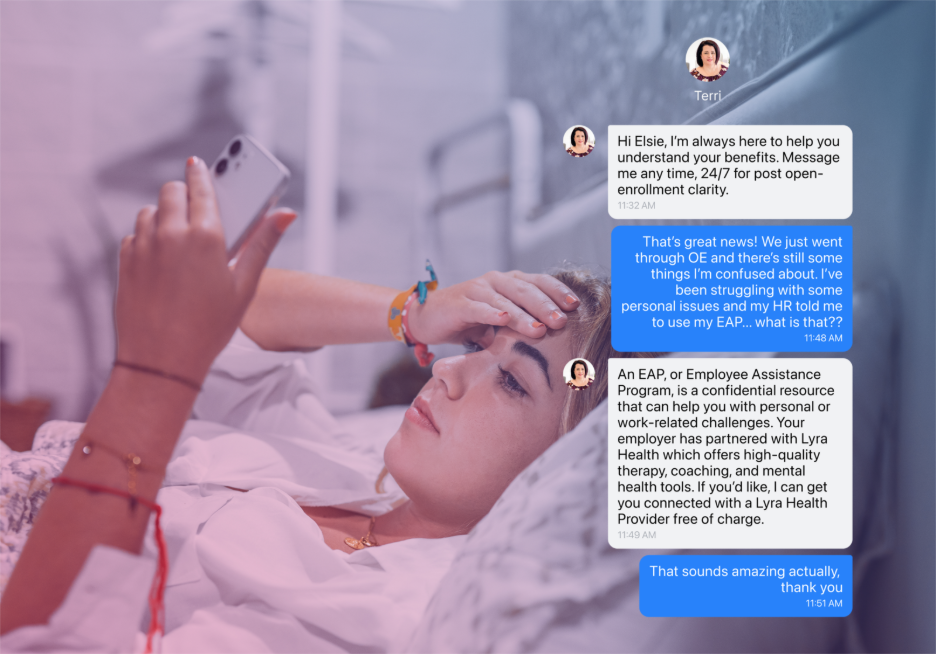
True engagement happens after enrollment, when employees are living their lives and making real healthcare decisions. They need clear guidance, reinforcement, and in-the-moment support— not a PDF they received months ago, sitting buried in their inboxes.
The most effective benefits strategies recognize this shift. They focus less on enrollment mechanics and more on what happens nxt, helping employees move from selection to confident use. This is where Medefy fits in: bridging the gap between enrollment and utilization by combining intuitive technology with human guidance when nuance, empathy, and clarity matter most.

By supporting employees with care navigation technology year-round, organizations can reduce confusion before it escalates, take pressure off of HR teams, and finally realize the value of the benefits they already offer.
January isn’t just a post-OE checkpoint— it’s a reset. A chance to ask a more meaningful question than whether or not employees simply enrolled. Do your employees actually know how to use what they chose?
Employers and brokers who address thatquestion early in the year set themselves up for stronger plan utilization, less HR burnout, and better outcomes long before the next renewal season arrives.
Open enrollment may be over. But theopportunity to improve benefits engagement is just beginning.